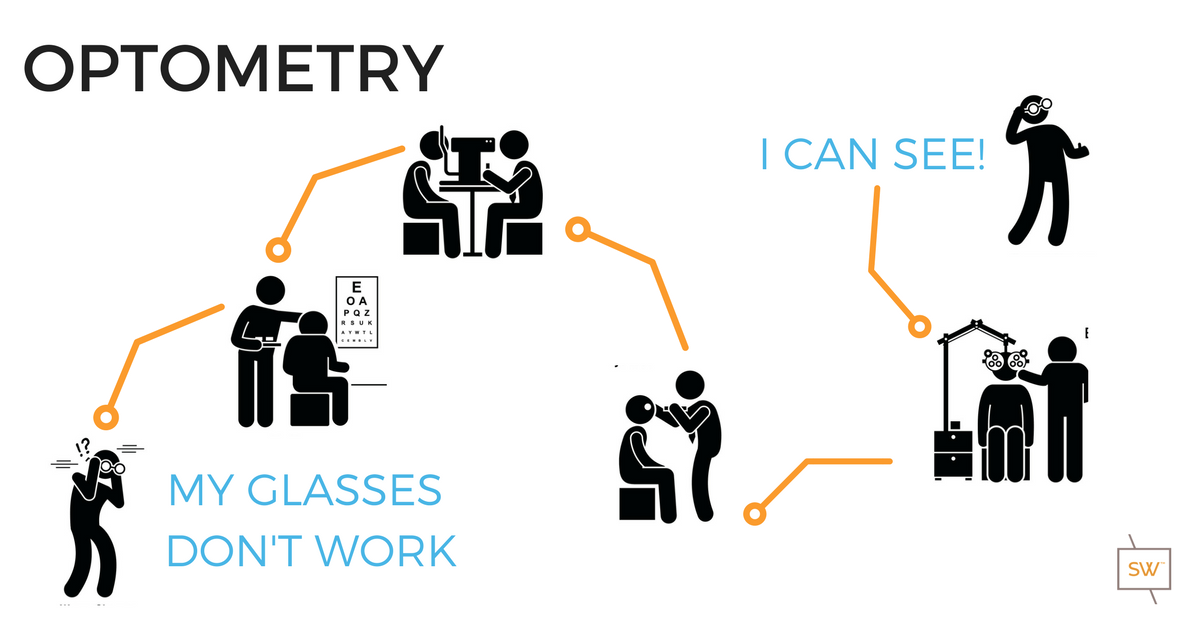
What Does an Optometrist Do All Day? Glasses....Glasses....Glasses....or....
/Have you ever wondered what an optometrists does all day?
Most people know that if they are experiencing blurry vision, they can visit an optometrist who will provide them with a prescription for glasses or contacts. But did you know that your optometrist does much more during your eye exam than merely prescribing glasses? And that not every cause of blurred vision can be fixed with glasses? That’s why every comprehensive eye exam also includes a thorough health check of your eyes. Why do your eyes need a health check? And what exactly is your Optometrist looking for?
For us to be able to see, light must travel into and through the eye without difficulty, from front to back. When light enters your eyes, it must pass through several layers before reaching the back of the eye, where visual information is then sent to your brain via the optic nerve.
Your Optometrist needs to examine all of these anatomical layers to evaluate your eye's ability to receive and appreciate the light. To do this, they use an instrument called a "slit lamp", which utilizes a series of lenses and mirrors to magnify your eye, similar to a microscope.
The health of your eyes can change at any time and can be happening without you knowing it. The only way to be sure that your eyes are healthy is to have regular eye health checks. Most optometrists would recommend yearly eye health checks, just like your medical doctor and dentist do.
So what exactly is your optometrist looking for
during these health checks?
Let's start by reviewing the anatomy of your eyes!
The outermost layer of the eye is called the cornea. Many people confuse the cornea with the iris, which is the coloured part of the eye. The cornea is crystal clear and needs to stay that way to optimize the movement of light through its layers. The shape of the cornea is also partly responsible for determining the prescription of your glasses and contacts. For example, if your cornea is not perfectly spherical in shape, then you likely have some degree of astigmatism. Infections and scratches can cloud the cornea, causing a decrease in your vision. The cornea is protected by a tear film layer that is left behind after each blink you take. A compromised tear film can lead to dry eye symptoms such sandiness and grittiness on the front of your eye.
Surrounding the cornea on all sides, the “white of your eyes” is called the sclera. This area is a tough outer layer that acts like a shell to protect the eye from puncture. You might notice that the sclera appears red from time to time. This redness is due to the enlargement of blood vessels sitting on top of the sclera. These blood vessels are normally very thin and difficult to see but become enlarged as a reaction to irritation. This irritation can be caused by many things, including infection, inflammation and dryness.
Sitting behind the cornea is the iris or “coloured part of the eye”. The colour of the iris ranges from dark brown to pale blue depending on the amount of pigmentation present: a tremendous amount of pigment in brown eyes, a tiny bit of pigment in green eyes, and almost no pigment at all in blue eyes! In the middle of the iris, there appears to be a round black dot. However, this dot is actually a hole known as the pupil. You may have noticed that the size of the pupil changes throughout the day. This is normal. The pupil size will be large in dim lighting and small in bright lighting. It is the job of the iris to respond to the surrounding light levels with the appropriate pupil size for optimal vision. Inflammation of the iris, called iritis or uveitis, can affect the function of the iris, and lead to pain and light sensitivity.
Sitting behind the iris is the crystalline lens. "Crystalline" because it is crystal clear the day you are born. Just like the cornea, the lens needs to remain as transparent as possible to allow us to see the world around us. The lens is made up of collagen, is very flexible, and natural movements within the lens allow us to read. The lens becomes less flexible with time, and consequently, our reading ability gets weaker and weaker as we age. Decreased lens flexibility leads to the eventual need for reading glasses or progressive lenses. If the lens becomes cloudy or opacified in any way, whether by ageing, systemic conditions, or as a side effect of certain medications, it becomes what is known as a cataract. A cataract can significantly block the light travelling through the eyes and lead to a decrease in vision.
Sitting between the crystalline lens and the back surface of the eye is the vitreous humour. The vitreous is colourless and clear. It is a jelly-like tissue that is 99% water. The remaining 1% is made up of collagen, proteins, salts, and sugars. The vitreous provides protection to the eye as well as helps it to keep its spherical, or ball-shaped, appearance. With time, the collagen and proteins become "stringy", and the vitreous begins to liquefy. This creates symptoms of "floaters" which are more noticeable when looking at a white wall or a blue sky. Sometimes various health conditions necessitate the removal of the vitreous humour, and this is done through a process known as a "vitrectomy".
Once the light moves from the outside world, through the cornea, into the pupil and through the crystalline lens and vitreous humour, it finally hits the retina. The retina is where all the millions of receptors and nerves that convert the light into vision is located. Therefore it needs to be checked very carefully by your optometrist who will assess the macula, the optic nerve head, the blood vessels, and all other areas of the retina.
The macula is densely packed with photoreceptors and is responsible for your central, high-resolution vision. Damage to the macula can permanently affect your vision, and even cause blindness. Common causes of damage to the macula include smoking cigarettes and excessive sunlight exposure, which can lead to macular degeneration. The macula can also be damaged by uncontrolled diabetes. Permanent loss of vision due to damage to the macula can result in loss of one's driver's license and limited job opportunities.
The optic nerve is a collection site. Photoreceptors from the entire retina carry information to the optic nerve head, which is a direct line from the eye to the brain. Nerve damage from glaucoma is visible at the optic nerve head. Another important problem to rule out is papilledema, or swelling of the optic nerve head. This can cause headaches, blurred vision, and signal possible swelling within the brain itself.
The blood vessels carry oxygenated blood and nutrients to the retina to maintain optimal function. Many systemic problems such as diabetes and high blood pressure can disrupt these blood vessels. It is important that your optometrist assess the blood vessels for leaks and proper blood flow.
Let's look at a few case examples, where your optometrist does a little more then you might think
Case Study 1:
Debbie Johnson goes to her optometrist, Dr. McKenzie, complaining of pain when opening and closing her left eye. Her left eye is also red and watery. Her right eye feels perfectly fine. Dr. McKenzie uses his slit lamp to examine her cornea. He notices a thin, whitish line on her cornea. It looks like a corneal abrasion, or scratch to the front of the eye. He then uses an orange dye called Sodium Fluorescien to help highlight the cornea and confirms that it is indeed a corneal abrasion
A corneal abrasion is an open wound to the eye and therefore can become infected if not treated. Dr. McKenzie starts Debbie on a course of antibiotics eye drops to fight any infection and to allow the cornea to heal itself. He may also prescribe lubrication eye drops to aid in comfort. It is important to discontinue any contact lens use while the cornea heals.
Case Study 2:
Ben West goes to his optometrist, Dr. Lim, complaining of cloudy vision. He says it has been steadily getting worse over the last year and now he is noticing changes in his colour vision as well. Dr. Lim uses her slit lamp to evaluate his eyes. She notices a problem with the crystalline lens and recommends dilating Ben's eyes to get a better look at the lens as well as the retina to determine the cause of Ben's complaints. Once Ben's eyes are fully dilated from the diagnostic drops, Dr. Lim uses her slit lamp again. She notices that the crystalline lens has turned light brown in colour. No problems are found at the retina.
Ben's blurry vision and colour vision problem are due to cataracts and Ben will be sent to an Ophthalmologist for cataract surgery. Cataracts cause blurry vision that cannot be corrected by glasses and surgery becomes a necessity to continue daily tasks at the same level as before.
Case Study 3:
John Jackson goes to his optometrist, Dr. McKenzie, complaining of warped central vision in his right eye. When he looks at something, like a tree, the trunk looks bent and distorted. Dr. McKenzie is very concerned about John's macula based on his complaint and recommends a dilated eye exam. 20 minutes after the dilation drops go in, Dr. McKenzie uses his slit lamp and a high plus lens to examine the macula of John's right eye. He sees a distortion of the macula and fluffy, yellow spots surrounding the macula.
John has signs and symptoms of macular degeneration. John needs to begin taking daily vitamins specially designed to aid the macula and fight off degeneration. If the degeneration continues to progress, John may need surgical intervention such as monthly injections. There are many risk factors that predispose someone to develop macular degeneration. These include excessive sun exposure, smoking, and a fair complexion.
Another common cause of John's symptoms is a macular hole. This can be caused by tugging of the vitreous body on the macula. This may or may not need surgical treatment, but if it does, John may need a vitrectomy, which is a removal of the vitreous body to alleviate the tugging on the macula.
Case Study #4
Pamela Clark goes to her optometrist, Dr. Randhawa, complaining of a veil-like curtain over her left eye. She is also seeing flashes of light from the corner of her eye and increased number of floaters. Dr. Randhawa is very concerned about Pamela's retina based on her complaints and recommends a dilated eye exam. Once her eye is fully dilated, Dr. Randhawa uses her slit lamp to exam the retina of Pamela's left eye. Dr. Randhawa sees a small horseshoe-shaped tear in the outer retina. Pamela has a retinal tear, and emergent surgery is needed. Dr. Randhawa sends Pamela to the nearest hospital for surgery. Retinal tears and detachments can cause a permanent loss of vision and require immediate attention. It is important that anyone experiencing flashes or floaters be assessed right away by an optometrist.
Case Study 5:
Jane Fields goes to her optometrist, Dr. McKenzie, complaining of watery eyes throughout the day. Dr. McKenzie uses his slit lamp to exam the front surface of the eye and sees dry corneas. Jane's watery eyes are related to dry eye. This seemed counter-intuitive to Jane as her eyes are too wet, not too dry, but Dr. McKenzie explains to her that her cornea signals to the brain that it is dry and the brain responds by signalling to her glands to produce more tears. That is why a dry eye is a watery eye. Dry eye can be caused by many things including wind and a low humidity environment. It is helpful to wear sunglasses outside as well as to supplement with artificial tears.
Hopefully, this has given you an insight into the things your optometrist is looking for every time you come in for an eye exam.
Your eye health is essential to the function of your eye and needs to be examined on a regular basis.
BOOK YOUR NEXT EYE EXAM IN EDMONTON
WITH A STONEWIRE OPTOMETRIST